The Basics
So what is cath lab?
The "cath lab" is short for catheterization laboratory. Catheterisation is the medical procedure where a thin, flexible tube called a catheter is inserted into a body cavity, duct, or vessel for various purposes, including diagnosis, treatment, or drainage. In the context of the cath lab, catheterisation refers to the minimally invasive procedure to diagnose and treat cardiovascular diseases using catheters.
Why "lab"? In medicine, "laboratory" doesn't always refer to a space solely dedicated to scientific research. It also denotes a specialized room equipped for specific procedures or tests.
A bit of history...
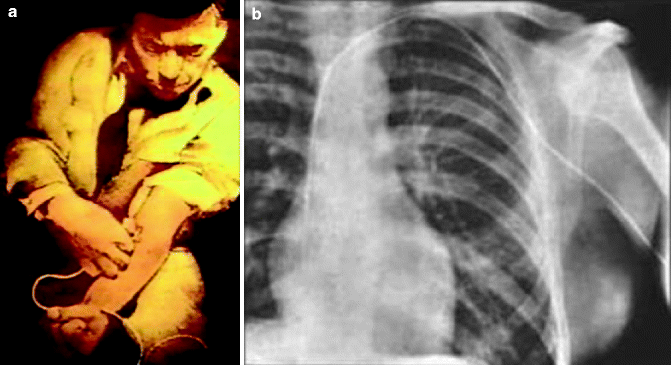
In 1929, Werner Forssmann performed the first human cardiac catheterization on himself by inserting a catheter into his own antecubital vein (as in the img below) and advancing it toward his right atrium. To verify its position, he walked to the radiology department and used X-ray imaging to take a fluoroscopic image of the catheter reaching his right atrium. Other key milestones include the introduction of right heart catheterisation (cardiac output and pulmonary pressures) by Mason Sones and Dickinson Richards in 1945, the first balloon angioplasty by Andreas Grüntzig in 1977, and the development of stents in the 1980s.
Who's in the cathlab?
Everyone has their own responsibilties in cathlab. As always, it is our responsibility to work together as a team and assist each other when needed to improve workflow and ultimately better outcomes for the patient.
- Doctors (2)
- Fellow: Cardiologists who have completed general training and are now specialising and advancing their skills in interventional studies. Typically the main physician performing the examinations.
- Consultant: Fully qualified cardiologists who have extensive experience in the cathlab. Typically sit outside the lab and give direction to the fellows. Decisions are ultimately based on their advice.
- Registrar: Not as often in the labs, junior doctors who usually start off by performing diagnostic LHCs (no PCI). May not be as quick and need assistance with the equipment/common errors!
- Nurses (2-3)
- Scrub: Assist the cardiologist in the procedure.
- Scout: Assist with various tasks such as opening sterile packages, communicating with the pt and scribing.
- Cardio physiologists or techs (1)
- Monitor patients' vital signs, operate specialized equipment (e.g. IVUS) and scribe during procedure. Typically sit outside the lab by the door.
- Radiographers (1)
- Assist with C-arm control, screen displays and imaging related tasks (e.g. referencing, image labelling, radiation safety).
- PSAs
- Assist with pt transfer and turnover as well as transporting pts if required.
- Echocardiologists
- Present when TOE is used e.g. TAVI, mitral-clip insertion.
- Confirm presence of abnormalities in the heart structure or clots prior to beginning procedures.
- Anaesthetist
- Present for GA/heavy sedation cases, intubated pts from ICU or ED and when airway support is required.
- May also assist with TOE in certain cases.
- Medical device reps
- More commonly present in TAVI and EP studies, assisting the doctors and nurses with new and emerging devices / trial cases!
What are the different start times?
- 8:00am - Put pedals out for the labs which are running (look at the whiteboards and check EMR) and check rooms are ready (e.g. plastic covers on lead shielding). Turn on LCD/inside screens (using smaller touch-screen next to Sony Screen) and CR screens (white wall switches). Put armboards on table if LHC first exam/radial access.
- 8:15am - Main start time, see supervisor and get assigned a lab.
- 9:00am - [Float] Start in x-ray and call cath lab to see if you are needed.
- 9:30am - See supverisor and usually begin relieving people for breaks starting with the 8:00am person. Finish the day by checking all labs are cleaned and machines/screens turned off.
- 4:00pm - Typically need to head up to the labs at 4:30 to finish any cases still going on (usually CRM labs 6/7).